Eligibility & Enrollment

The Alameda Health Consortium’s Eligibility and Enrollment Department provides our member community health centers with training, resources, and technical support.
What
Alameda Health Consortium coordinates eligibility and enrollment efforts with our member health centers through training, resources, and technical support.
Why
To help ease the complex navigation process of enrolling community members in social safety-net programs.
How
By facilitating enrollment through four major programmatic components.
Read More

Individuals applying for Medi-Cal and CalFresh through community health centers receive extensive assistance from health center staff who provide expertise and understanding of the eligibility and enrollment criteria. Enrollment staff help explain how to complete the application criteria, collect required documentation, and prepare for County eligibility review and disposition. Additionally, health center staff assist Medi-Cal and CalFresh beneficiaries with their annual renewals, so that they do not lose their health coverage.
Alameda Health Consortium works with more than 90 certified enrollment counselors across our community health centers, by coordinating enrollment efforts, tracking changes in Medi-Cal CalFresh, Covered California health plans, and HealthPAC, and by providing ongoing training and technical assistance to health center staff.
May is CalFresh Awareness Month!
CalFresh, known federally as the Supplemental Nutrition Assistance Program or SNAP, provides monthly food benefits to individuals and families with low-income and provides economic benefits to communities. CalFresh is the largest food program in California and provides an essential hunger safety net. CalFresh is federally mandated and in California, is state-supervised and county-operated.
Read More
CalFresh benefits can help buy nutritious foods for a better diet. CalFresh benefits stretch food budgets, allowing individuals and families to afford nutritious food, including more fruit, and vegetables. The amount of benefits a household receives is dependent on household size, countable income, and monthly expenses, such as housing and utilities. The program issues monthly benefits on an Electronic Benefit Transfer (EBT) card. Food may be purchased at any grocery store or farmer’s markets, or restaurants that accept EBT cards.
How Can I Apply for CalFresh?
-
- Community Health Centers
- BenefitsCal
- Social Services Agency
- GetCalFresh.org
- Call 1-877-847-3663 (FOOD)
Additional CalFresh Resources
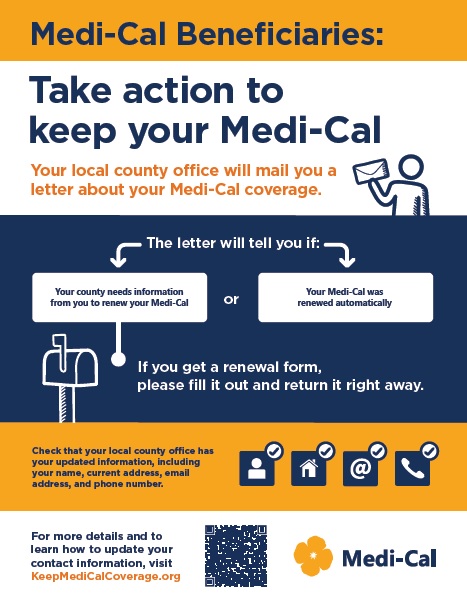
 Medi-Cal Coverage
Medi-Cal Coverage
Medi-Cal is California’s Medicaid Program. It is a health care coverage program for low-income families and individuals who live in California. Since March 2020, Medi-Cal renewal processing was put on hold due to the continuous coverage requirement, as a result beneficiaries retained their Medi-Cal coverage with no renewal process.
As of April 2023, Alameda County Social Services Agency resumed the Medi-Cal renewal process. Keep yourself and your family covered.
Read More
Ensure that your information is updated, check your mail, and complete your Medi-Cal renewal packet and return to the County office by the due date in order to avoid a break in coverage.
-
- Statement of intent
- Keep your Medi-Cal
- Medi-Cal coverage toolkit
- Alameda County: Keep your Medi-Cal Flyers
- General: Keep your Medi-Cal Flyers
For more information on Eligibility and Enrollment please email: eligibilitygrants@alamedahealthconsortium.org

