HealthPAC Funding Needs to Remain Intact
The Health Program of Alameda County, also known as HealthPAC, is a county program that provides affordable health care to uninsured people living in Alameda County. In addition to funding healthcare services and emergency transportation for uninsured patients, HealthPAC also supports quality and system improvement efforts across the board as well as collaboration between our member health centers.
Periodically we’ll be highlighting how HealthPAC funding has been used by our member health centers. We recently sat down with our member health center Asian Health Services to talk about what the consequences could be if HealthPAC funding is no longer available for their patients, both uninsured and insured.
Alameda Health Consortium: What does HealthPAC funding mean for your health center?

Asian Health Services: HealthPAC funding is a key source of stable funding that enables Asian Health Services (AHS) to provide care to its uninsured population, ensure top quality services, and support our patients’ continuous eligibility, enrollment and renewal into important health programs that have helped to target and address many of the health inequities our patients often face. HealthPAC has provided critical financial stability for AHS, particularly during the pandemic.
HealthPAC ensures that AHS has the support and capacity to enroll and renew patients into the CalFresh program – AHS
It enabled AHS to successfully transition to telehealth, which was a key lifeline for our patients, and supported us during the pandemic. While we did not directly use HealthPAC funding for COVID response efforts, HealthPAC funding was critical in that it provided us with the ability and stability to rapidly pivot and respond during COVID-19 pandemic in such a way that we did not have to furlough or lay off any staff.

With HealthPAC funding, our Hepatitis programs have greatly improved the health of our patients who are both diagnosed with chronic Hepatitis and at-risk of Hepatitis. Hepatitis B infections disproportionately impact the Asian community. With HealthPAC funding, AHS can support three Provider Champions – one at each of AHS’ three largest sites. These providers have been successful in providing culturally competent Hepatitis universal screenings and treatments for our patients in the diverse Asian languages that our patients speak that have resulted in transformative and impactful patient outcomes. Given that Provider Champions provide on-site expertise, peer support and training to other Providers, Provider Champions have been a critical element to the success of this program and has enabled AHS to be a national model for Hepatitis initiatives focused on underserved populations.

HealthPAC funding has also been critical in supporting no-cost medications to all of our uninsured patients under 200% of FPL. In addition, HealthPAC ensures that AHS has the support and capacity to enroll and renew patients into the CalFresh program while enabling patient access to monthly food distributions at the local park.
AHC: Beyond assisting with uninsured patients, what are some of the projects/innovations HealthPAC has helped fund that you’re the proudest of?
AHS: We were able to leverage HealthPAC funding to initiate a Remote Patient Monitoring (RPM) Project. Our RPM project was a critical intervention during the pandemic since our patients faced not only COVID, but also anti-Asian hate. Given this “dual” pandemic, our patients feared being attacked or assaulted when coming into the clinic, yet it was important for our most chronically ill to receive continuous care (care during, after, and between medical appointments).
Knowing that healthcare professionals are working closely with us, monitoring readings, and communicating with us regularly – we feel comforted and at ease – SHIP Patient, Ko Lim Lee

In response, AHS was able to leverage HealthPAC funding to start the Smart Hypertensive Improvement Project (SHIP). The SHIP Program focused on AHS’ highest risk hypertensive patients, and utilized an innovative approach to managing their care, where patients were given smart (Bluetooth) connected blood pressure cuffs and a smartphone (if they did not have one already). Patients could take their own blood pressure readings, sync them to an app on their smartphone, and transmit the data to AHS’ medical providers and care teams. The SHIP Program has been tremendously successful since AHS first piloted it in early 2021. The SHIP program has also shown great success in controlling patients’ blood pressure. Of patients engaged in SHIP, an impressive 90% have either controlled or improved their blood pressure readings over the past 30 days.
Watch this video to learn more about AHS’ Remote Blood Pressure Monitoring System
We also established a Technology Hub to support patients in utilizing telehealth and technology for RPM and help to close the digital divide gap. These technology hubs will provide Tech 101 workshops in different Asian languages and will provide support to patients who need help troubleshooting their phones, computers, or laptops. AHS’ patients, particularly its immigrant elders who speak little to no English and have little to no technology literacy, are often greatly challenged to access virtual care due to these digital divide challenges. In fact, many patients have never used a computer or the internet, and many more have never had a smart phone. Most patients rely on the younger generation or relatives for help accessing technology.

AHS would like to deploy additional in-language Digital Health Advocates (DHA) to provide in-language assistance for patients to overcome digital divide barriers. DHA’s can support patients in utilizing remote patient monitoring devices, connecting to the internet, and using virtual and telehealth tools. They will also provide translation/interpretation where needed, and can refer patients to the medical team for urgent issues. Since telehealth will continue beyond the pandemic, we will continue to expand remote patient monitoring as a standard mode of care.
AHC: What are the gaps in access to care that HealthPAC funding is currently helping to fill?
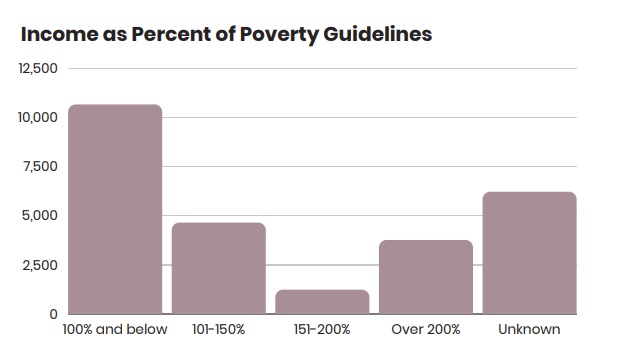
AHS: Given the Health Resources and Service Administration (HRSA) requirement of sliding fee scale discounts (co-pays and deductibles) for privately insured patients, we have been able to utilize HealthPAC funds to improve access to care for both our uninsured and underinsured patients (including privately insured patients) whose incomes are below 200% FPL. HealthPAC funds also support our efforts to provide medications at no charge to uninsured and underinsured patients up to 200% of FPL.
AHC: What happens to these gaps if this funding is no longer available?
AHS: We are facing unprecedented pressure to increase staff wages at all levels. At the same time, the reimbursement for care has not kept pace with inflation. HealthPAC funding has been a stabilizing force for AHS during the pandemic. As a critical and stable funding source, it is enabling AHS to recover from the fiscal and workforce repercussions that have occurred from the pandemic.
If funding is no longer available, we will have less resources to support our most chronically ill patients, who are in need of tailored, culturally competent, language accessible programming and services. Without sustainable funding, there could be possible staffing cuts, and the chasm of health care inequities and disparities created by the dual pandemic of COVID and anti-Asian hate will widen.
It is critical that HealthPAC funding stay intact at the current level, especially during this time with increasing inflation and labor costs and when workforce recruitment, retention and well-being are significant challenges. Should HealthPAC funding levels drop or if funding is no longer available, additional obstacles and barriers that could be created are AHS holding off on expanding additional services as well as thinking about the real possibility of reinstating co-pays for medications. This would be a huge step back for us as a community health center that has strived to carve a concrete path towards health equity. HealthPAC funding must remain intact.
Learn more about Asian Health Services HERE.
