The Alameda Health Consortium’s Healthcare Access Department provides our member community health centers with training, resources, and technical support.![]()
Alameda Health Consortium works with more than 90 certified enrollment counselors across our member community health centers throughout the East Bay, by coordinating enrollment efforts, tracking changes in Medi-Cal CalFresh, Covered California health plans, and HealthPAC, and by providing ongoing training and technical assistance to health center staff.
Medi-Cal
Medi-Cal is California’s Medicaid Program It is a healthcare coverage program for low-income families who live in California. For most people – Medi-Cal is not changing. Most Medi-Cal members will keep the same eligibility and benefits.
The following groups can keep their Medi-Cal with dental coverage and will not have to pay a monthly premium, regardless of immigration status.
- Children ages 0-18 years old
- Current and former foster youth under age 26 years old
- Pregnant individuals
Read More
Covered benefits include seeing your doctor and going to the hospital or getting emergency care. Medi-Cal members will still be able to fill their prescriptions, get mental health supports, and receive treatment for substance use.
Other services still covered will be regular checkups, shots or vaccines, long-term care, non-emergency medical transportation, dental and vision care.
You will still be able to access the healthcare benefits and services you need to maintain and support your health.
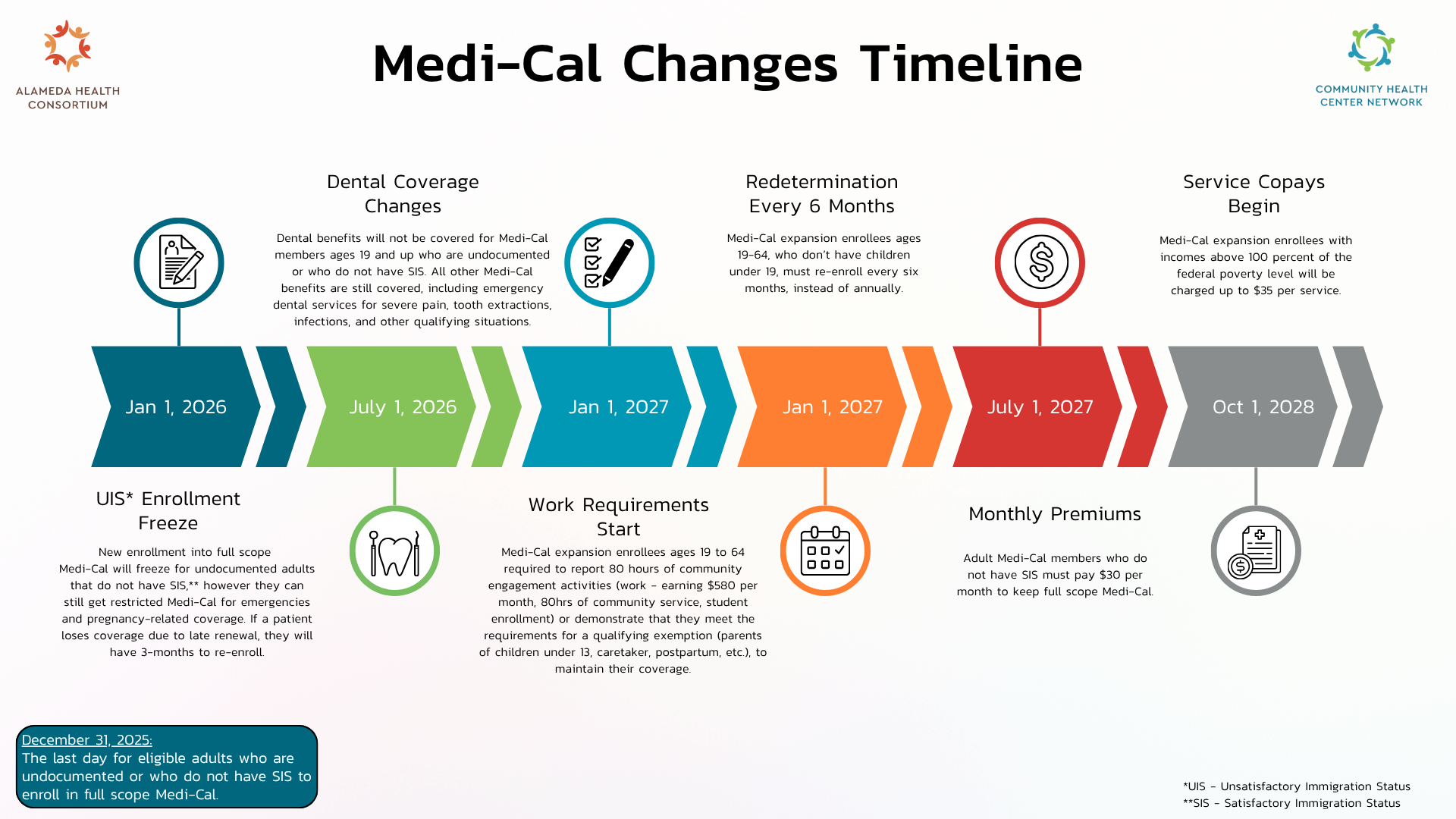
The Health Consumer Alliance (HCA) has put together a snapshot of each of these upcoming changes below.
A detailed timeline with more information on each of the upcoming changes to Medi-Cal can be found on the Department of Healthcare Services, Medi-Cal Program Changes page – What Medi-Cal Members Need to Know or by clicking the Learn More buttons below.
Additional information, provided by DHCS, regarding immigration status and Medi-Cal Eligibility can be found here.
For more information on Eligibility and Enrollment please email: eligibilitygrants@alamedahealthconsortium.org
CalFresh

CalFresh, known federally as the Supplemental Nutrition Assistance Program or SNAP, provides monthly food benefits to individuals and families with low-income and provides economic benefits to communities. CalFresh is the largest food program in California and provides an essential hunger safety net. CalFresh is federally mandated and in California, is state-supervised and county-operated.
Read More
CalFresh benefits can help buy nutritious foods for a better diet. CalFresh benefits stretch food budgets, allowing individuals and families to afford nutritious food, including more fruit, and vegetables. The amount of benefits a household receives is dependent on household size, countable income, and monthly expenses, such as housing and utilities. The program issues monthly benefits on an Electronic Benefit Transfer (EBT) card. Food may be purchased at any grocery store or farmer’s markets, or restaurants that accept EBT cards.
How Can I Apply for CalFresh?
-
- Community Health Centers
- BenefitsCal
- Social Services Agency
- CalFresh Benefits Info Line: Call 1-877-847-3663 (FOOD)
Covered California

Individuals applying for Medi-Cal and CalFresh through community health centers receive extensive assistance from health center staff who provide expertise and understanding of the eligibility and enrollment criteria. Enrollment staff help explain how to complete the application criteria, collect required documentation, and prepare for County eligibility review and disposition. Additionally, health center staff assist Medi-Cal and CalFresh beneficiaries with their annual renewals, so that they do not lose their health coverage.
Visit the Covered California Navigator Program to learn more about the federally mandated state health exchanges HERE.
